The Global Cancer Burden: Avoidable Causes from Lifestyle to Environment
David Schottenfeld
John G. Searle Professor Emeritus and Former Chair of Epidemiology and Professor Emeritus of Internal Medicine
The causes of cancer are legion, but a sober look at dominant risk factors here and abroad can help maximize limited resources in our fight against this deadly disease.
A key insight from cancer prevention data in recent decades is just how different that fight looks from country to country. Indeed, the global cancer burden exhibits strikingly different patterns in industrialized high-income countries and low- and middle-income countries (LMICs).
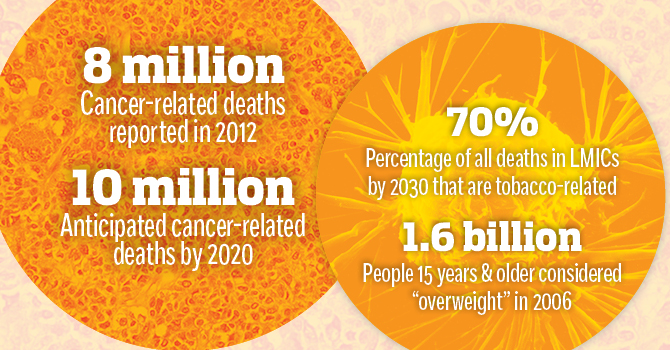
In 2012, the World Cancer Report estimated that there were approximately 14 million cancer cases and 8 million cancer-related deaths. By 2020, based on population aging and growth, and age-specific mortality rates, the projected global cancer mortality will exceed 10 million cancer deaths, or that 15% of global deaths will be attributed to cancer.
Approximately two-thirds of global cancer deaths occur in LMICs that comprise 80% of the world's population. That number is projected to increase due to factors like urbanization, sedentary lifestyles, and rises in chronic disease that contribute to cancer risk. Behavioral and environmental risk factors include increasing use of various forms of tobacco, obesity, and exposures to cancer-causing infectious agents.
Recent studies estimate that eight lifestyle and environmental risk factors—tobacco, alcohol, obesity, physical inactivity, cancer-causing infectious agents, occupations, ionizing and solar radiations, and dietary consumption of red and processed meats—account for 50% of population cancer mortality. The proportion of global cancer cases attributable to infectious agents has been estimated between 16–17%, exceeding 2 million cases per year.
An important synergy occurs when exposure to alcohol is combined with tobacco.
Tobacco. In the five decades since the 1964 Surgeon General's report on Smoking and Health, much has been learned about the global tobacco epidemic. In the US and in many countries of Western Europe, tobacco consumption peaked in the 1960s and 1970s, then declined as tobacco control programs were motivated by evidence linking tobacco and cancer. In LMICs, if current trends in smoking patterns continue, tobacco-related cancer deaths will double by 2030, with 70% of deaths occurring in LMICs.
Alcohol. Chronic alcohol consumption and its carcinogenic compound acetaldehyde have been associated with risk of cancers of the mouth and throat, liver, intestines, breast, and pancreas. An important synergy occurs when exposure to alcohol is combined with tobacco. In the US and many industrialized countries, the percentage of total cancer incidence attributable to excessive alcohol consumption is around 4–5% in men and 1–2% in women. The lowest alcohol-attributed cancer risks are in the Middle East and North and Sub-Saharan Africa.
Physical Inactivity and Obesity. The World Health Organization (WHO) estimated in 2006 that 1.6 billion persons aged 15 years and older were "overweight," of whom 400 million were classified as "obese." Excess body weight has been established as an avoidable cause in 5–8% of cancer cases in the US (primarily colorectal, esophageal, pancreas, postmenopausal breast, and endometrial cancers). In managing the global epidemic of obesity, the WHO has emphasized the complexity of social, cultural, and economic factors that influence food preferences, energy intake, and energy expenditure. New research on genetic and metabolic mechanisms regulating fat distribution, endocrine and immune system functioning, and other factors will continue to improve our ability to control obesity-related cancer patterns.
Cancer-Causing Infectious Agents. The fraction of cancers attributable to infectious agents varied from 20–30% in LMICs, in contrast to 5–10% in highly industrialized countries. Infections caused by the bacterium Helicobacter pylori, hepatitis B virus, hepatitis C virus, and the human papillomaviruses accounted for more than 90% of cases attributable to infectious agents.
Occupations. Most recognized occupational carcinogens have been identified through studies of men in high-income countries. Studies in European countries have estimated that 3–5% of cancer deaths in men and 1–2% of cancer deaths in women may be attributed to occupational causes. In the US, 2.5–4.8% of cancer deaths were attributed to occupational causes. The cancer sites prominently associated with occupational exposures are urinary bladder, bone marrow, lung, pleura/peritoneum (mesothelioma), sinonasal, and liver (angiosarcoma). Prominent chemical exposures include asbestos, silica dust, benzene, diesel engine exhaust, radon, and rubber manufacturing.
Mitigating the global and US burden of cancer mortality is possible by integrating population-wide preventive measures targeting these primary causes. And the role of public health will continue to be crucial in this massive endeavor.
This article first appeared in the spring 2018 issue of Findings, the magazine of the University of Michigan School of Public Health.
About the Author
David Schottenfeld is John G. Searle Professor Emeritus and Former Chair of Epidemiology and Professor Emeritus of Internal Medicine. He helped found the American Society of Preventive Oncology and has been designated as a fellow of the American College of Physicians, the American College of Preventive Medicine, and the American College of Epidemiology. Schottenfeld and colleague Joseph Fraumeni, former Director of the Division of Cancer Epidemiology and Genetics of the National Cancer Institute, are co-authors of Cancer Epidemiology and Prevention, the world's leading textbook on the subject now in its fourth edition.
